Search by category, archive or keyword

If people on the street were asked to name the most important organ of the human body, the organs cited most frequently would likely be the heart, brain, and lungs.
The liver, however, is considered the most important organ according to some experts, including well-known medical personality Dr. Oz. It is not surprising that the liver ranks so high in importance among medical professionals, given its detoxifying, infection-fighting, energy-storing, and digestive abilities.
The hard-working liver labors tirelessly in the right upper quadrant of our abdomen, and given its low-key nature (no throbbing, pulsing, or breathy sounds), it’s easily forgotten. In fact, the liver rarely causes pain in the absence of a serious condition. Knowing the earliest signs and symptoms of liver disease is imperative in seeking timely medical treatment and intervention.
Facts About Liver Disease
According to the American Liver Foundation, at least 10 percent of Americans have some form of liver disease. Additionally, the American Liver Foundation reports that hepatitis C, non-alcoholic fatty liver disease, and liver cancer are all occurring with greater incidence.
Alcohol abuse, hepatitis viruses, and obesity – all considered highly preventable – are the leading three risk factors for death from liver disease. Other causes of liver disease include cancer, autoimmune diseases, and genetic or metabolic disorders.
Sadly, symptoms of many liver disorders do not manifest until serious – sometimes irreversible – damage has occurred. A population-based study found that 69 percent of adults with cirrhosis were unaware of having liver disease. Another study found that Hispanic Americans and African Americans are at greater risk for developing liver disease than Caucasians.
Hispanic Americans have a greater risk due to heavier drinking and a higher prevalence of obesity and diabetes, while African-Americans have a higher prevalence of obesity, diabetes, and hepatitis B or C.
Non-Alcoholic Liver Disease
When people refer to liver diseases or damage not caused by excessive alcohol use, they’re usually referring to a non-alcoholic fatty liver disease, also known as NAFLD. This condition leads to excess fat gathering in the liver.
Damage caused by NAFLD presents signs and symptoms similar to liver disease by alcohol abuse. Non-alcoholic fatty liver disease is an umbrella term, with the most common form simply named fatty liver. Causes of fatty liver include:
- Obesity
- Diabetes
- High levels of fat in the blood
Fatty liver usually does not have symptoms and is reversible with lifestyle changes.
A more advanced NAFLD condition is non-alcoholic steatohepatitis (NASH). In this condition, fat growth is associated with liver cell inflammation and varying degrees of scarring to the organ. NASH is a serious condition and may lead to severe scarring of the liver as well as cirrhosis.
Alcoholic Liver Disease
Many people have heard of the signs and symptoms of alcoholic liver disease, such as jaundice (yellowing of the skin and whites of the eyes), fatigue, and digestive issues.
Less commonly known signs and symptoms of alcoholic liver disease include:
- Skin conditions such as itchiness, eczema, and psoriasis
- Bad reactions to medications such as antibiotics or pain relievers
- Frequent heartburn and acid reflux
Additionally, alcohol abusers might notice significant decreases in their alcohol tolerance, becoming inebriated more quickly than usual. Alcohol abusers might also suffer more severe hangovers than usual as liver disease develops.
What does Alcohol do to your Body?
Alcohol, although legal and socially acceptable, arguably has the most profound impact on the human body, both mentally and physically. Alcohol has an effect on many different organs, such as the liver, pancreas, stomach, and esophagus. Alcohol use can cause malnutrition and vitamin deficiencies such as low thiamine. Low thiamine is often found in Wernicke-Korsakoff syndrome, a condition that causes mental deterioration, often referred to as ‘wet brain.’
Most notably, alcohol use can have life-threatening effects on the liver. Many alcoholics have an elevated Bilirubin which is responsible for the normal breakdown of red blood cells. Other liver problems are the destruction of liver cells and cirrhosis – scarring of the liver.

Alcohol is a central nervous system depressant and affects everything from the liver to the heart. It is thought that alcohol and benzodiazepines are the most common substances of abuse that cause death both during use and during detoxification and withdrawal.
Much time is spent on discussing and researching how alcohol affects the person consuming alcohol. What about its Teratogenic effects? Fetal alcohol syndrome occurs when an unborn fetus is affected by the mother’s consumption of alcohol.
Some of the damage caused is slower than normal body growth and development, palpebral fissures, underdeveloped facial bones, and a very thin and fine upper lip. Alcohol use during pregnancy can also cause problems later in life for the child, such as cognitive issues and maladaptive behaviors.
Stages and Early Symptoms of Liver Disease among Alcoholics
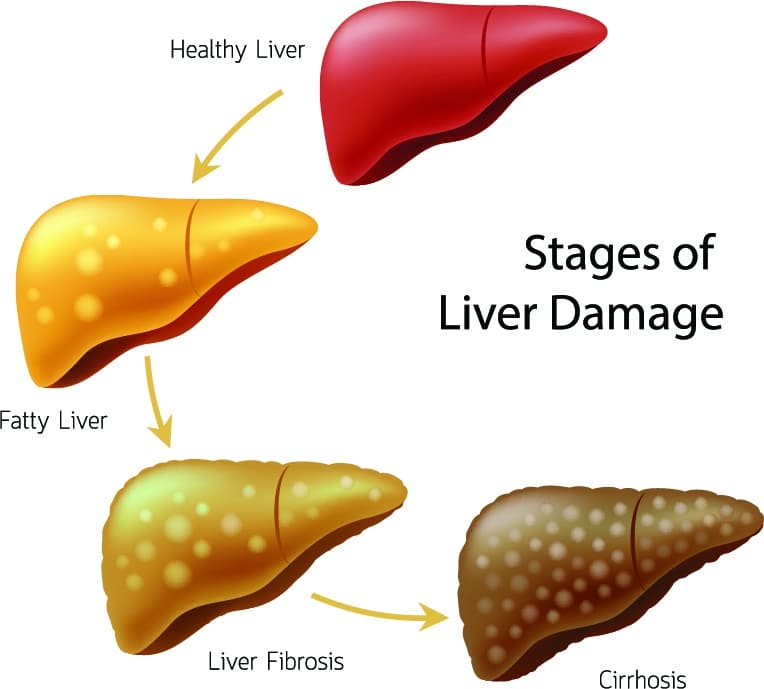
The American Liver Foundation names three types of alcoholic liver disease. These are – in order of most to least severe – alcoholic cirrhosis, alcoholic hepatitis, and alcoholic fatty liver disease. The signs and symptoms of these may overlap.
Alcoholic Fatty Liver Disease
This disease happens when fat builds up in the liver, which causes swelling and impairs liver function. Alcoholic fatty liver disease can occur even after a short period of heavy drinking.
Symptoms are not usually present in this stage, though the American Liver Foundation reports some may feel weak or fatigued or notice discomfort in the right upper abdomen but the damage is still occurring within the liver tissues
With the cessation of alcohol use, drinkers can usually reverse liver disease in this stage. If drinking continues, damage to the liver will not subside and will result in irreversible disease.
Jaundice
Jaundice, the yellowing of the skin or eyes, is the result of excess bilirubin in the body. During the course of normal blood production, the body produces bilirubin excreted by the liver. When the liver sustains damage from alcohol use, it is unable to excrete bilirubin, causing the pigmented substance to build up in the body.
People with jaundice may also experience abdominal pain, flu-like symptoms, and fatigue. The presence of jaundice itself is non-life-threatening, but it often signals an underlying issue with the liver itself.
Alcoholic Hepatitis
This condition can manifest after long-term drinking. This involves inflammation and scarring of the liver, which prevents blood flow in the organ, slowing its essential functions. Even though alcoholic hepatitis might be diagnosed as “mild,” it is a serious condition requiring abstinence from adult beverages.
Severe alcoholic hepatitis can be life-threatening. Left untreated, it can progress to cirrhosis of the liver. Alcoholic Steatohepatitis is a severe form of hepatitis that affects up to 20% of heavy drinkers and can lead to permanent damage and scarring.
The mildest forms of alcoholic hepatitis might not present any signs or symptoms. As the condition advances, signs and symptoms might include:
- Jaundice
- Fatigue
- Low-grade fever
- Loss of appetite
- Nausea
- Vomiting
- Tenderness in the right upper abdomen
- Weight loss
Liver function tests will also reveal elevated liver enzymes. Severe alcoholic hepatitis may lead to abdominal fluid accumulation, cognitive and behavioral changes, and liver or kidney failure. It is imperative you seek medical advice and intervention at this stage.
Alcoholic Cirrhosis
This condition is not reversible, though abstinence from alcohol may prevent further damage and improve some signs and symptoms. In this type of liver disease, severe scarring of the liver is present.
People with alcoholic cirrhosis will almost certainly be dependent on alcohol and require medical treatment and a great deal of support. This scar tissue makes it difficult for the liver to perform its functions properly.
Likewise, people with cirrhosis may experience inflammation of the liver leading to abdominal pain, fat buildup in the liver cells, redness of the palms, shortening and thickening of the fingers, and more. A person suffering from alcohol-related cirrhosis who continues to drink has less than a 50 percent chance of living for five more years.
You cannot live without your liver
The liver is a crucial organ that most of us never think about … unless it fails. By the time a liver stops functioning, it’s too late, and the only real option is hoping you draw the golden ticket for a transplant. Alcoholic liver disease is a serious and potentially fatal disease. Non-alcoholic liver disease can have the same prognosis.
Read More: What to do when an Alcoholic Doesn’t want help
Whether liver disease develops from alcoholic or non-alcoholic causes, it is important to be aware of the early signs and symptoms. Early detection is the best chance of stopping the damage before the organ stops functioning completely.
Liver Spotting
One sunny Tuesday morning, Sonya woke up yellow.
Like normal Tuesday mornings, she put her kids on the school bus and dressed herself for work. But as she began to apply her light-beige foundation, she abruptly stopped. What she saw in the mirror was anything but normal. Her face, arms, and neck were yellowed.
Jaundice is just one of the many symptoms of liver damage. And it can come on suddenly.
Since we can’t see when ugly liver spots develop or the organ discolors or show abnormalities, we must rely on other methods to spot trouble.
Symptoms and Signs to be Wary of for Liver Disease
New research is finding new molecules that may offer new treatments in a cure for liver disease. Experiments, tests, and treatments are continually being explored. Still, the best treatment is early detection.
Your quiet liver does more than you might think, like fighting infection and storing energy.
Some of the signs of early liver damage include:
- Irregular sleep
- Low or fluctuating energy levels
- Skin and eyes developing a yellowish tint
- Skin conditions appear, such as eczema, psoriasis, acne, and itching
- Drinking minimal amounts of alcohol inebriates quickly and causes intense hangovers
- The impact of caffeine becomes acute
- Flushing from the trunk rising up to the head
- Experiencing severe reactions and side effects to common medications
When early liver damage creeps up, the body can no longer protect against harmful chemicals. The body stops being able to digest food, remove impurities, filter toxins from the blood and send nutrients where they need to go.

The declining liver also presents with these signs:
- Bleeding or bruising easily
- Stomach problems after eating, such as bloating, gas, and nausea
- Frequent headaches, heartburn, and acid reflux
- Difficulty losing weight or inexplicable weight gain
- A strange urinary smell after eating asparagus
- Chemicals (bleach, perfume, gasoline, paint, cleaning products) cause a severe reaction
In addition to the symptoms of non-alcoholic liver damage, those with alcoholic liver damage often experience tremors.
Amazing Regrowth of the Liver
Bob has an old army injury in his knee that developed arthritis. He took pain medicine for years until, suddenly, he got very sick. After a year’s journey of illness and treatments, Bob received a liver transplant.
Since the human liver regenerates and can return to its original size, Bob’s partial liver failure meant he could receive a partial liver transplant from a living donor.
Bob’s lifespan potential has been increased due to receiving a transplant and the amazing regenerative properties of the liver. However, liver transplants are not easy to come by. There are currently thousands of people on the national waiting list for a hepatic transplant.
The liver has the ability to grow back when damaged, and the body can heal itself in small ways. Lifestyle changes like eliminating alcohol, drugs (including too much Tylenol-containing medications), tobacco, and seeking nutritional therapy can enhance the liver’s natural healing abilities.
Only people who have abstained from all alcohol for a period of at least six months can be considered for a transplant. In addition, all other organs must be healthy, and the individual must be able to undergo surgery. Since alcohol dependency can affect other organs, this may affect an alcoholic’s ability to be considered for a liver transplant as well.
Even with a hepatic transplant, the rate of survival after one, three, and five years declines, respectively.
Non-Alcoholic Liver Damage
Non-alcoholic fatty liver disease is unrelated to alcohol and refers to excess fat gathering in the liver.
Non-alcohol-related liver disease can be brought on by:
- Inflammation due to an injury or infection
- Hepatitis
- Obesity
- Cancer
- Malnutrition
- Poison
- Medication overdose
- Genetic disorders
- Autoimmune failure
- Diabetes
Non-alcoholic liver damage goes through the same stages as an alcohol-damaged liver. It is the cause of the disease that differs.
Alcoholic Liver Damage
Wanting to give up alcohol? Advanced medical tests, research studies, and scientific knowledge put together a picture of what quitting alcohol can do for avoiding or halting liver damage.
Alcohol abuse is one of the primary causes of liver damage. Alcohol-associated liver disease is the main cause of chronic liver disease in Western countries.
Once you are diagnosed with alcoholic liver damage, there is one key factor:
Abstaining from alcohol is the only chance a person has of recovery.
Stages of Alcoholic Liver Disease
Alcohol drains the body of nutrients, affects many organs, and damages tissues.
There are four main stages of alcoholic liver disease, each one worse than its predecessor.
Alcohol Fatty Liver Disease
Heavy drinking can cause fatty acids to collect in the liver, in some cases in less than a week.
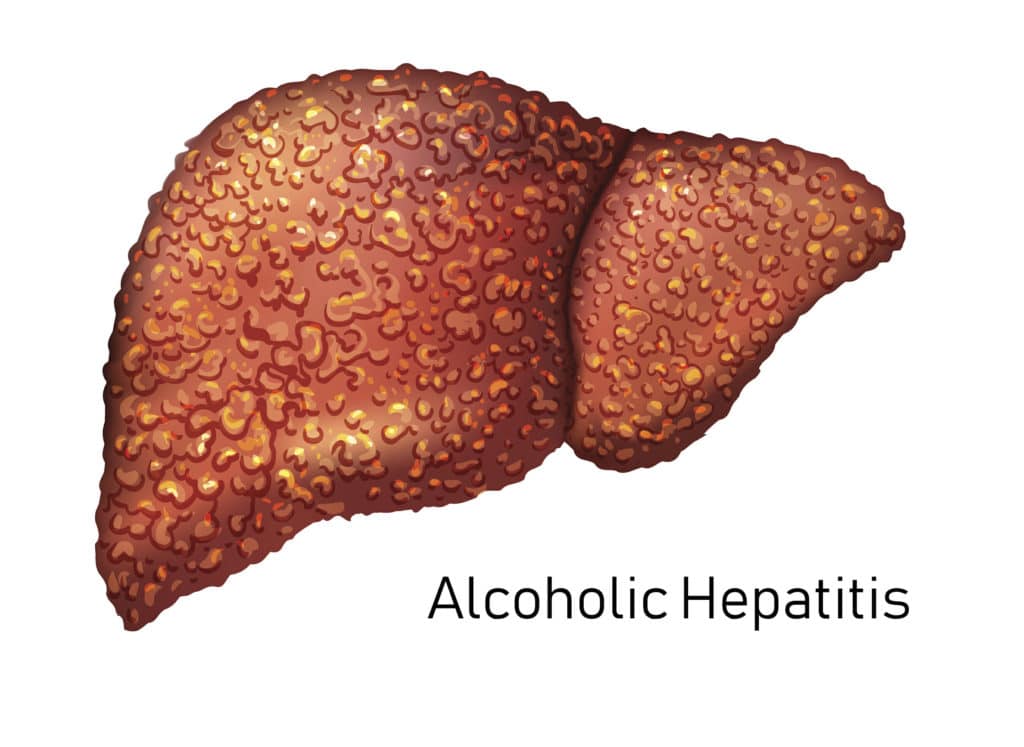
Alcoholic Hepatitis
After years of heavy drinking or acute periods of binge drinking, the liver can develop inflammation and swelling. This swelling and inflammation of the liver are known as hepatitis.
Other types of hepatitis can cause non-alcoholic liver disease.
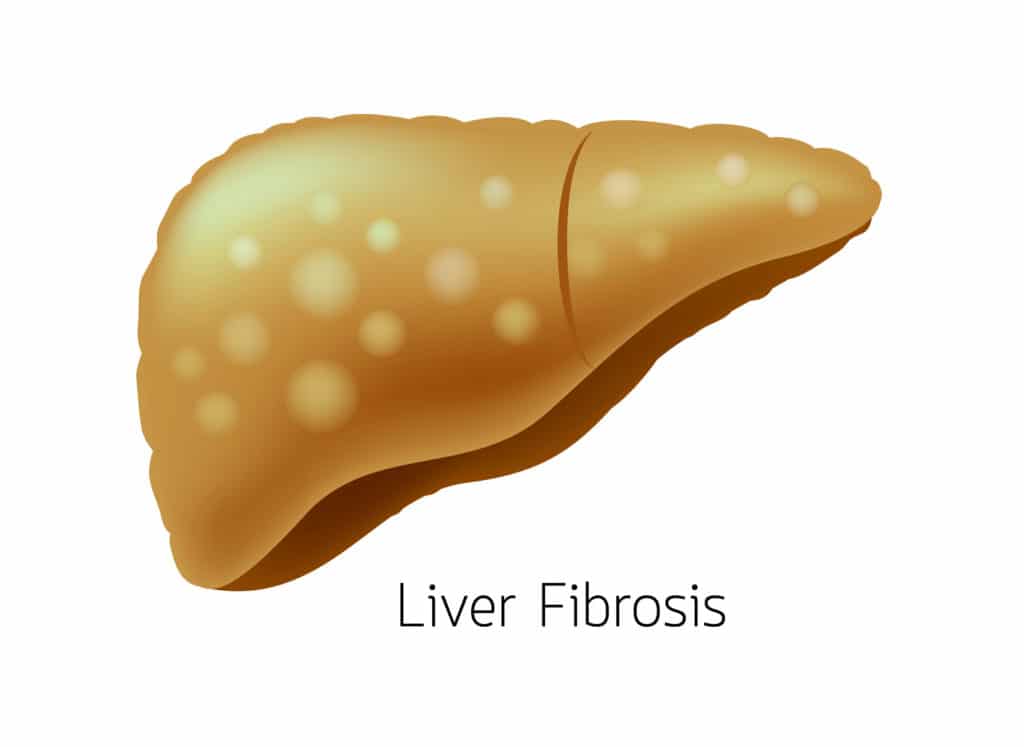
Alcoholic Fibrosis
The third stage of liver disease is fibrosis, a buildup of proteins in the liver. Instead of filtering toxins and breaking down proteins, the liver accumulates too many proteins, resulting in fibrosis.
The newest research indicates gut microbiota play an influential role in liver injury. As we learn more and more about gut-brain health and gut-liver health, researchers point out the abilities of alcohol cessation and dietary and supplement improvements to slow the progression of liver disease.
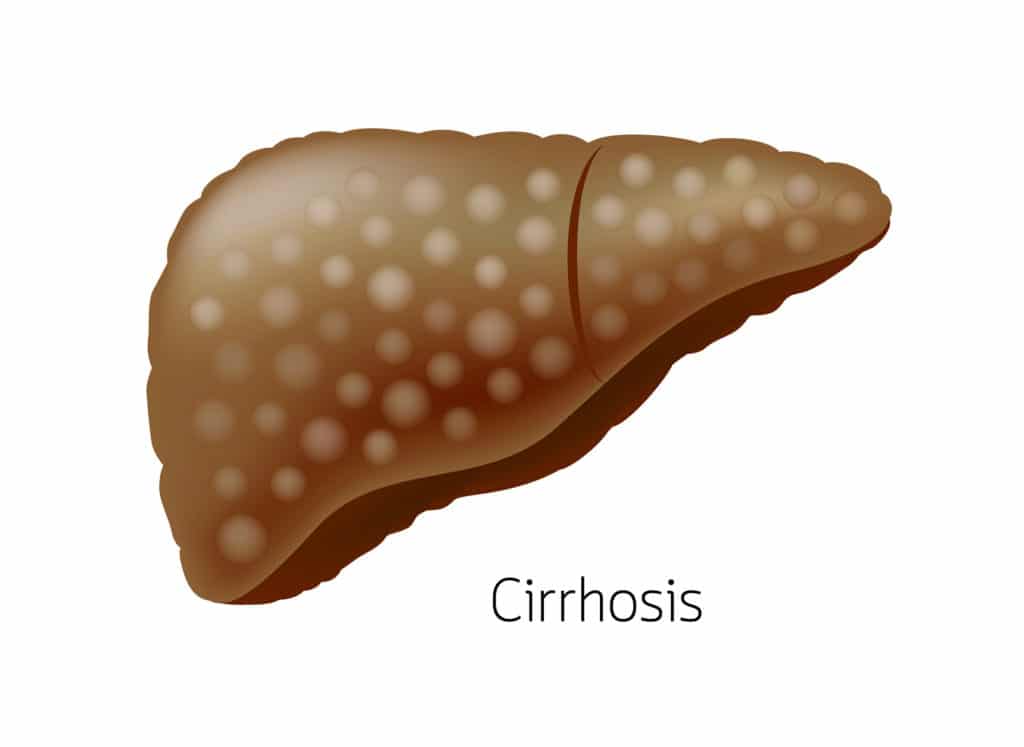
Alcoholic Cirrhosis
Cirrhosis of the liver is scarred tissue that takes over healthy tissue.
When the liver has been inflamed for a long time, cirrhosis occurs. This is the stage where the loss of function happens. Cirrhosis can lead to liver cancer and end-stage liver disease.
Alcohol use speeds up the destruction of the liver and reduces its ability to compensate for damage.
Can you Reverse Liver Damage from Alcoholism?
The human body has an amazing capacity to heal itself. At the same time, a limit exists for what it can do. The human body can reverse damage from several types of minor liver damage; however, in some cases, the damage might be permanent. If you can reverse liver damage from alcoholism, it will occur in the earliest stage of dependency.
Cirrhosis is permanent, and you cannot undo the damage that has already occurred. Scarring is permanent, and the liver has lost its previous ability to function normally. However, a healthy lifestyle can help mitigate the risk of further damage.
In other cases, such as fatty liver disease, you can reverse the damage from alcohol. The liver has the benefit of being the body’s only regenerative organ. In fact, if you lost 75% of your liver, it would regenerate to its previous size. When Alcohol Liver Disease (ALD) is in its early stages, it is possible to heal the liver and restore its functioning completely. Improving liver health will require adherence to a healthy lifestyle and a dedication to feeling your best.
How Long Does It Take the Liver to Regenerate?
The liver is a vital organ that has the ability to heal itself, even after years of heavy drinking. In the event that 50-60% of the liver cells die, then the liver should be able to regenerate within 30 days. However, it’s important to recognize that good liver health is an ongoing effort that requires adherence to a healthy lifestyle.
Consequences of Drinking Too Much
Noteworthy, anything that jeopardizes the amazing regenerative ability of the liver puts your life in danger.
The further liver disease progresses, the more dangerous it becomes.
A 29-year-old Californian, Brandon didn’t think he was an alcoholic. After his family held an intervention, Brandon realized his weekend binge drinking was a serious problem. When he went to rehab, his medical team found signs of liver disease, and tests confirmed the diagnosis.
Thankfully, Brandon’s condition was discovered early enough that the holistic and medical treatments he received arrested the damage. Two years later, the young man’s scans showed significant improvement, and thanks to the support he received, Brandon has stayed sober.
Out of mind while chugging down beers and liquors, developing alcoholic liver disease can quickly become life-threatening for anyone.
According to the American Liver Foundation, between ten and twenty percent of heavy drinkers will develop alcoholic liver cirrhosis from repeated and excessive alcohol use.
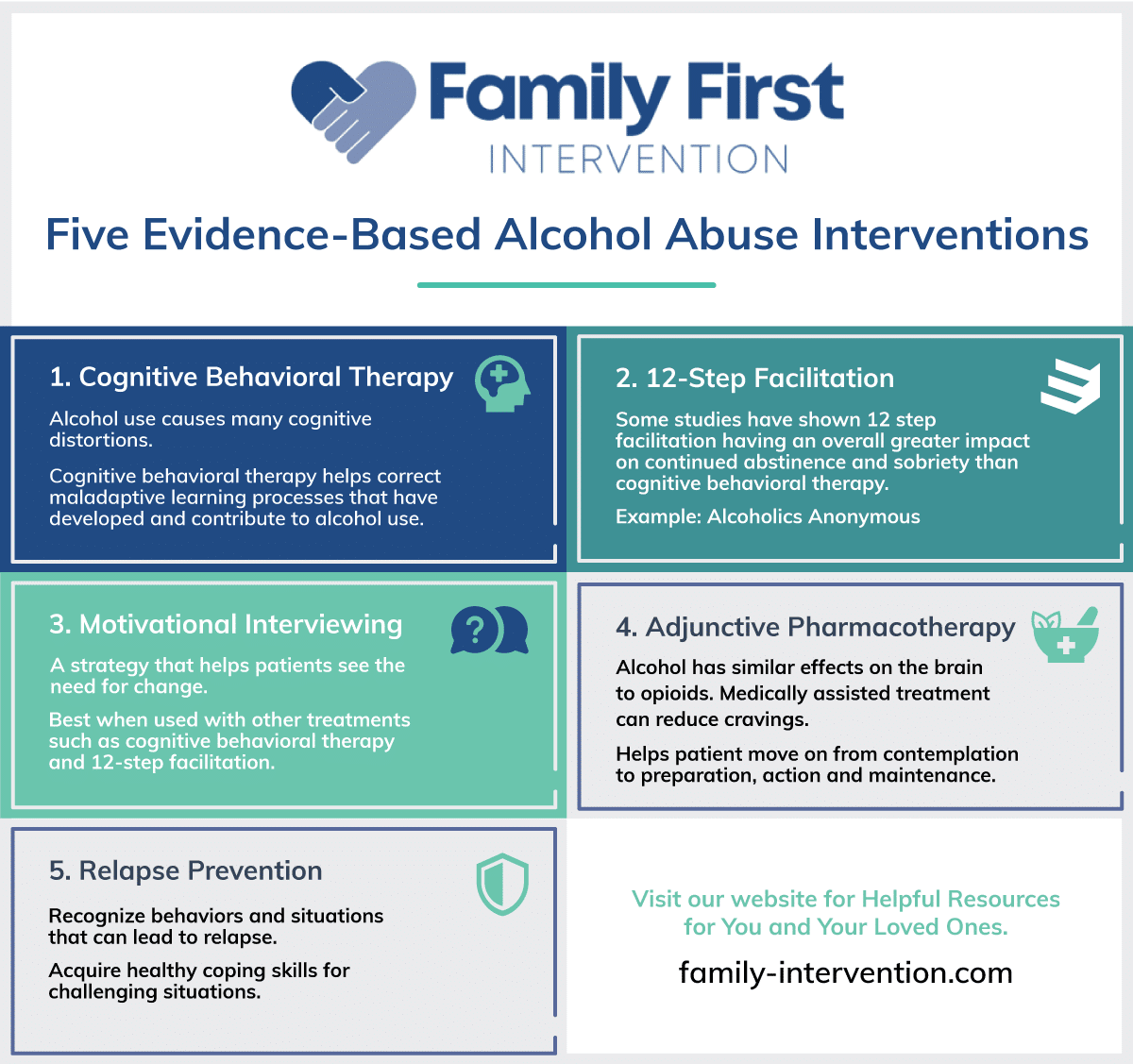
Five Evidence-Based Alcohol Abuse Intervention
Cognitive Behavioral Therapy – Cognitive behavioral therapy is an evidence-based treatment that can be very effective in the treatment of alcohol use disorder. Alcohol use causes many cognitive distortions. Cognitive behavioral therapy helps correct maladaptive learning processes that have developed and contribute to alcohol use.
12-Step Facilitation – Yes, groups like Alcohol Anonymous are effective evidenced-based treatments for alcohol use disorder. In fact, some studies have shown 12-step facilitation having an overall greater impact on continued abstinence and sobriety than cognitive behavioral therapy.

Adjunctive Pharmacotherapy – Medications such as Naltrexone have been shown to reduce cravings in a number of patients with alcohol use disorder. Alcohol has similar effects on the brain to opioids. Medically assisted treatment shows greater efficacy when used in conjunction with other treatments, such as cognitive behavioral therapy and 12-step facilitation.
Motivational Interviewing – MI is a strategy used by clinicians to help the patient with alcohol use disorder see the need for change. When facilitated effectively, motivational interviewing can help the patient move on from the contemplation stage of change into the stages of preparation, action, and maintenance.
Relapse Prevention is designed to assist the patient in recognizing high-risk behaviors and situations that can potentially lead to relapse. Relapse prevention techniques often include acquiring healthy coping skills to help a substance user navigate through any challenges they may face. Relapse prevention discussion and strategy are often discussed during one’s stay in treatment and again as part of their discharge planning.
Help for Signs of Early Liver Disease
The recommended daily limits for alcohol consumption are no more than one drink per day for women and two for men.
If you or someone you know regularly exceeds these recommended daily limits or is experiencing some early signs of liver disease, it is important to intervene early.
Medical treatment for addiction recovery is vital. Quitting alcohol is a formidable challenge, and withdrawing from alcohol at home can be life-threatening.
Getting a professional intervention early on is a person’s best chance of reversing the strain alcohol puts on the liver. Let us help today.
This was originally posted on October 19, 2016, and was updated and updated January 26, 2022
An intervention is not about how to control the substance user; it is about how to let go of believing you can.
“The most formidable challenge we professionals face is families not accepting our suggested solutions. Rather, they only hear us challenging theirs. Interventions are as much about families letting go of old ideas as they are about being open to new ones. Before a family can do something about the problem, they must stop allowing the problem to persist. These same thoughts and principles apply to your loved one in need of help.”
Mike Loverde, MHS, CIP